Tendinosis: History, Histopathology, Pathogenesis, Evaluation, and Treatments of the underreported chronic tendon condition.
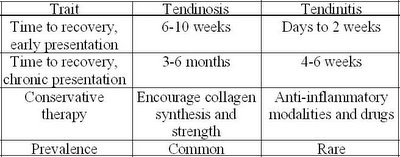
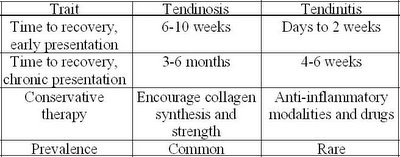
The term tendinosis was first used in the 1940’s by a group of German researchers, however the term did not receive much attention until it was used again in the mid 1980’s to describe a non-inflammatory tendon condition. The more commonly used term of ‘tendinitis’ has since been proven to be a misnomer for several reasons. The first of which is that there is a lack of inflammatory cells in conditions that were typically called a tendonitis. Since inflammation is the key pathological process involved with that term, and the discovery that there in fact were no, or very few, inflammatory cells present in the condition, a new term was adopted – tendinosis. This has a much greater impact then just the name one calls a condition, it also has a profound impact on how the condition is treated. Khan compares the time to recovery of an acute and chronic presentation of tendinosis versus tendonitis, as well the prevalence and focus of conservative therapy. They are outlined as follows:
Histopathology of Tendinosis
A typical healthy tendon is composed of primarily type I collagen with minimal amounts of type III collagen interspersed within the neatly arranged parallel fiber orientation of type I collagen. The healthy tendon is said to be white and shiny and reflect polarized light under microscope. Unhealthy tendons, or tendinosis, appear gray and do not reflect polarized light under the microscope. As previously mentioned, there are no inflammatory cells found in the collagen of chronic tendinosis conditions, there may however be a few chronic (not acute) inflammatory cells present if there is healing of a partial tear of the tendon. There are however three key findings present in tendinosis conditions. They are: disrupted collagen fibers within the tendon, increased cellularity, and neovascularization.
Kraushaar and Nirschl found that on cross section of collagen, an area of tendinosis showed that the collagen was of variable diameter, uneven mixture of thick and thin fibrils and in some areas did not even connect with each other to form a tendinous structure. They concluded that the ultrastructure of collagen in tendinosis is unable to sustain a tensile load. Maffulli et al. confirmed these findings and also discovered that the collagen that is formed in an area of tendinosis is actually type III collagen, instead of the predominant type I in healthy tendon. This increase in type III collagen, and possible decrease in type I collagen results in a decrease in the forces that the tendon can withstand and may eventually lead to tendon rupture.
The other two findings present in tendinosis, increased cellularity and neovascularization has been termed angiofribroblastic hyperplasia by Nirschl. The cells present in tendinosis are mesenchyme-derived tendon fibroblasts (tenocytes) and myofibroblasts, as opposed to the humoral process of an immune based inflammatory response. These are cells that represent a degenerative condition. Khan described the types of degeneration associated with tendinosis as either mucoid or lipoid. Mucoid degeneration causes softening of the area affected as well as the characteristic changes seen in tendon from the glistening white appearance to the gray appearance in tendinosis. Lipoid degeneration is characterized by an abnormal increase in lipid material in a tendon.
Neovascularization found in tendinosis has been described as a haphazard arrangement of new blood vessels and Kraushaar et al. even mention that the vascular structures do not function as blood vessels. Vessels have even been found to form perpendicular to the orientation of the collagen fibers. They then concluded that the increased vascularity present in tendinosis is not associated with increased healing.
Pathogenesis
Tendinosis is said to be a degenerative condition affecting a tendon. The cause of this degeneration has been thought to be due to one of several things, of which overuse causing microtrauma appears to be the most widely accepted. Kraushaaar describes four stges of injury due to micro trauma. Stage-1 is said to be most likely inflammatory in nature and is associated with pathological alterations that most likely will resolve. Stage-2 injury is associated with pathological alterations such as tendinosis and angiofibroblastic degeneration. Stage-3 injury is associated with pathological changes (tendinosis) and complete structural failure (rupture). Finally, stage-4 injury exhibits features of both stages 2 and 3 along with other findings such as fibrosis, soft matrix calcification, and hard osseous calcification.
There is also said to exist a tendinosis cycle that must be broken before successful treatment and pain-free movements can be restored. The cycle of tendinosis is simplified and described as repetitive overuse activities or microtraumas causing microtears in the tendon creating a fibroblastic hyperplasia response, which then respond by increasing the amount of type III collagen within a tendon. This further weakens the tendon causing more microtears and prolonging the degenerative cycle.
Treatment for this condition must first attempt to stop the degenerative cycle and then to restore proper collagen synthesis, strength and function.

Conservative Management
Kraushaar et al. lists the primary goals of treatment of tendinosis as being pain control, preservation of motion, flexibility and strength, and the development of endurance over time. Since the exact cause of pain in tendinosis is not known, many theories have tried to explain the mechanism of pain in order to improve treatment. The original theory of pain is based back to the concept of tendonitis where inflammation is the source of pain. Since there are no inflammatory cells present in tendinosis, this theory no longer applies. The next theory to evolve was that it is the biomechanical changes that result in pain production. Since a disruption of collagen is painful in a ligament sprain, why can’t the disruption of the collagen fibers in a tendinosis also be the cause of pain? Khan argues this notion by comparing a few post surgical patients with patellar tendinopathy who experience pain against those who do not. He mentions that the area when visualized is indistinguishable between painful and pain-free subjects, thereby negating a relationship between pain and collagen status. The next theory involves a biochemical model of pain. It is hypothesized that certain unknown chemicals may be responsible for pain production within an area of tendinosis. Certain chemicals that are already proven to be pain stimulators are glutamate and chondroitin sulfate.
Traditional treatments involve the use of corticosteroid injections for the treatment of tendonitis. It has been proven that corticosteroid injections actually further the degeneration of tendons and increase the risk of recurrence of the condition as well as increase the risk of tendon rupture. That being said, corticosteroid injections have been shown to be effective in short term pain reduction for tendinosis. The mechanism is unclear but it is thought that bathing the area may alter or interfere with the local chemicals that cause the pain stimulus in the area.
Other treatments include biomechanical reduction of stress on the tendon, relative rest, and ice since it is a vasoconstrictor (and increased vascularity is a finding in tendinosis) and a natural analgesic. Research for the use of modalities such as laser and therapeutic ultrasound is controversial at best, however it is recommended by certain sources to help stimulate collagen synthesis. Stretching and strengthening are two common methods of treating tendinosis and eccentric strengthening is gaining popularity quite rapidly.
Khan states that eccentric strengthening results in a stimulation of mechanoreceptors in tenocytes to produce collagen and thereby help reverse the tendinosis cycle. Alfredson et al. used heavy load eccentric calf muscle training in the treatment of chronic Achilles tendinosis and the found that all 15 participants were back to their preinjury activities after the 12 week training period. They performed 3 sets of 15 repetitions, with both the knee straight and knee bent, twice daily for twelve weeks. They did not perform the concentric portion of the exercise with the injured leg, they relied on the healthy leg to return them to the starting position each time. A more recent study by Shalabi et al. found that eccentric strengthening of the gastrocnemius-soleus complex resulted in a decreased tendon volume and intratendinous signal when evaluated by MR imaging. They also concluded that the findings were associated with decreased pain scores on a VAS and is therefore an effective adjunct in the treatment of Achilles tendinopathies.
Take Home Points:
1. Chronic tendon injuries are degenerative in nature and NOT inflammatory.
2. Anti-inflammatory medications (NSAID’s) and/or corticosteroid injections can actually accelerate the degenerative process and make the tendon more susceptible to further injury, longer recovery time and may increase likelihood of rupture.
3. Heavy load eccentric strength training helps to increase the tensile strength of the tendon, increase the amount of Type I collagen and decrease the amount of ground substance thereby reducing tendon volume and helping restore the tendon to a healthy state.
References:
Alfredson, H., Pietila, T., Jonsson, P., Lorentzon, R. Heavy-Load Eccentric Calf Muscle Training For the Treatment of Chronic Achilles Tendinosis. AJSM. Vol. 26 (3), 1998. pp.360-366
Cook, JL., Khan, KM., Maffulli, N., Purdam, C. Overuse Tendinosis, Not Tendinitis: Part 2: Applying the new approach to patellar tendinopathy. The Physician and Sportsmedicine, Vol 28 (6), June 2000.
Khan, KM., Cook, JK. Overuse Tendon Injuries: Where does the pain come from? Clinical Sports Medicine
Khan, KM., Cook, JL., Kannus, P., Maffulli, N., Bonar, SF. Time to abandon the “Tendinitis” Myth: Pianful, overuse tendon conditions have a non-inflammatory pathology. BMJ. Vol. 324 16 March 2002. pp.626-627.
Khan, KM., Cook, JL., Taunton, JE., Bonar, F. Overuse Tendinosis, Not Tendinitis: Part 1: A new paradigm for a difficult clinical problem. The Physician and Sportsmedicine, Vol 28 (5), May 2000.
Khan, KM. Cool, JL., Bonar, F., Harcourt, P., Astrom, M. Histopathology of Common Tendinopathies: Update and implications for clinical management. Sports Medicine. Jun 27 (6), 1999, pp. 393-408.
Kraushaar, B., Nirschl, RP. Tendinosis of the Elbow (Tennis Elbow). The Journal of Bone and Joint Surgery. Vol 81-A (2), Feb. 1999.
Maffulli, N., Ewen, SWB., Waterston, SW., Reaper, J., Barrass, V. Tenocytes from Ruptured and Tendinopathic Achilles Tendons Produce Greater Quantities of Type III Collagen than Tenocytes from Normal Achilles Tendons: An in vivo model of human tendon healing. AJSM Vol 28 (4), 2000.
Shalabi, A., Kristofferson-Wilberg, M., Svensson, L., Aspelin, P., Movin, T. Eccentric Training of the Gastrocnemius-Soleus Complex in Chronic Achilles Tendiopathy Results in Decreased Tendon Volume and Intratendinous Signal as Evaluated by MRI. AJSM, Vol. 32 No. X, 2004
Disclaimer
This information is not intended to be a substitute for professional medical advice. You should not use this information to diagnose or treat a health problem or disease without consulting with a qualified health care provider. Please consult your health care provider with any questions or concerns you may have regarding your condition.Any attempt to diagnose and treat an illness using the information in this site should come under the direction of a trained medical practitioner. We accept no responsibility for any adverse effects or consequences resulting from the use of any of the suggestions or procedures in this site or related internet links. By using the information in this web site you are confirming that you understand this statement and that you accept all risk and responsibility.
All matters regarding your health should be supervised by your health care provider. All information provided in this site is for the purpose of education, not treatment.
The term tendinosis was first used in the 1940’s by a group of German researchers, however the term did not receive much attention until it was used again in the mid 1980’s to describe a non-inflammatory tendon condition. The more commonly used term of ‘tendinitis’ has since been proven to be a misnomer for several reasons. The first of which is that there is a lack of inflammatory cells in conditions that were typically called a tendonitis. Since inflammation is the key pathological process involved with that term, and the discovery that there in fact were no, or very few, inflammatory cells present in the condition, a new term was adopted – tendinosis. This has a much greater impact then just the name one calls a condition, it also has a profound impact on how the condition is treated. Khan compares the time to recovery of an acute and chronic presentation of tendinosis versus tendonitis, as well the prevalence and focus of conservative therapy. They are outlined as follows:
Histopathology of Tendinosis
A typical healthy tendon is composed of primarily type I collagen with minimal amounts of type III collagen interspersed within the neatly arranged parallel fiber orientation of type I collagen. The healthy tendon is said to be white and shiny and reflect polarized light under microscope. Unhealthy tendons, or tendinosis, appear gray and do not reflect polarized light under the microscope. As previously mentioned, there are no inflammatory cells found in the collagen of chronic tendinosis conditions, there may however be a few chronic (not acute) inflammatory cells present if there is healing of a partial tear of the tendon. There are however three key findings present in tendinosis conditions. They are: disrupted collagen fibers within the tendon, increased cellularity, and neovascularization.
Kraushaar and Nirschl found that on cross section of collagen, an area of tendinosis showed that the collagen was of variable diameter, uneven mixture of thick and thin fibrils and in some areas did not even connect with each other to form a tendinous structure. They concluded that the ultrastructure of collagen in tendinosis is unable to sustain a tensile load. Maffulli et al. confirmed these findings and also discovered that the collagen that is formed in an area of tendinosis is actually type III collagen, instead of the predominant type I in healthy tendon. This increase in type III collagen, and possible decrease in type I collagen results in a decrease in the forces that the tendon can withstand and may eventually lead to tendon rupture.
The other two findings present in tendinosis, increased cellularity and neovascularization has been termed angiofribroblastic hyperplasia by Nirschl. The cells present in tendinosis are mesenchyme-derived tendon fibroblasts (tenocytes) and myofibroblasts, as opposed to the humoral process of an immune based inflammatory response. These are cells that represent a degenerative condition. Khan described the types of degeneration associated with tendinosis as either mucoid or lipoid. Mucoid degeneration causes softening of the area affected as well as the characteristic changes seen in tendon from the glistening white appearance to the gray appearance in tendinosis. Lipoid degeneration is characterized by an abnormal increase in lipid material in a tendon.
Neovascularization found in tendinosis has been described as a haphazard arrangement of new blood vessels and Kraushaar et al. even mention that the vascular structures do not function as blood vessels. Vessels have even been found to form perpendicular to the orientation of the collagen fibers. They then concluded that the increased vascularity present in tendinosis is not associated with increased healing.
Pathogenesis
Tendinosis is said to be a degenerative condition affecting a tendon. The cause of this degeneration has been thought to be due to one of several things, of which overuse causing microtrauma appears to be the most widely accepted. Kraushaaar describes four stges of injury due to micro trauma. Stage-1 is said to be most likely inflammatory in nature and is associated with pathological alterations that most likely will resolve. Stage-2 injury is associated with pathological alterations such as tendinosis and angiofibroblastic degeneration. Stage-3 injury is associated with pathological changes (tendinosis) and complete structural failure (rupture). Finally, stage-4 injury exhibits features of both stages 2 and 3 along with other findings such as fibrosis, soft matrix calcification, and hard osseous calcification.
There is also said to exist a tendinosis cycle that must be broken before successful treatment and pain-free movements can be restored. The cycle of tendinosis is simplified and described as repetitive overuse activities or microtraumas causing microtears in the tendon creating a fibroblastic hyperplasia response, which then respond by increasing the amount of type III collagen within a tendon. This further weakens the tendon causing more microtears and prolonging the degenerative cycle.
Treatment for this condition must first attempt to stop the degenerative cycle and then to restore proper collagen synthesis, strength and function.

Conservative Management
Kraushaar et al. lists the primary goals of treatment of tendinosis as being pain control, preservation of motion, flexibility and strength, and the development of endurance over time. Since the exact cause of pain in tendinosis is not known, many theories have tried to explain the mechanism of pain in order to improve treatment. The original theory of pain is based back to the concept of tendonitis where inflammation is the source of pain. Since there are no inflammatory cells present in tendinosis, this theory no longer applies. The next theory to evolve was that it is the biomechanical changes that result in pain production. Since a disruption of collagen is painful in a ligament sprain, why can’t the disruption of the collagen fibers in a tendinosis also be the cause of pain? Khan argues this notion by comparing a few post surgical patients with patellar tendinopathy who experience pain against those who do not. He mentions that the area when visualized is indistinguishable between painful and pain-free subjects, thereby negating a relationship between pain and collagen status. The next theory involves a biochemical model of pain. It is hypothesized that certain unknown chemicals may be responsible for pain production within an area of tendinosis. Certain chemicals that are already proven to be pain stimulators are glutamate and chondroitin sulfate.
Traditional treatments involve the use of corticosteroid injections for the treatment of tendonitis. It has been proven that corticosteroid injections actually further the degeneration of tendons and increase the risk of recurrence of the condition as well as increase the risk of tendon rupture. That being said, corticosteroid injections have been shown to be effective in short term pain reduction for tendinosis. The mechanism is unclear but it is thought that bathing the area may alter or interfere with the local chemicals that cause the pain stimulus in the area.
Other treatments include biomechanical reduction of stress on the tendon, relative rest, and ice since it is a vasoconstrictor (and increased vascularity is a finding in tendinosis) and a natural analgesic. Research for the use of modalities such as laser and therapeutic ultrasound is controversial at best, however it is recommended by certain sources to help stimulate collagen synthesis. Stretching and strengthening are two common methods of treating tendinosis and eccentric strengthening is gaining popularity quite rapidly.
Khan states that eccentric strengthening results in a stimulation of mechanoreceptors in tenocytes to produce collagen and thereby help reverse the tendinosis cycle. Alfredson et al. used heavy load eccentric calf muscle training in the treatment of chronic Achilles tendinosis and the found that all 15 participants were back to their preinjury activities after the 12 week training period. They performed 3 sets of 15 repetitions, with both the knee straight and knee bent, twice daily for twelve weeks. They did not perform the concentric portion of the exercise with the injured leg, they relied on the healthy leg to return them to the starting position each time. A more recent study by Shalabi et al. found that eccentric strengthening of the gastrocnemius-soleus complex resulted in a decreased tendon volume and intratendinous signal when evaluated by MR imaging. They also concluded that the findings were associated with decreased pain scores on a VAS and is therefore an effective adjunct in the treatment of Achilles tendinopathies.
Take Home Points:
1. Chronic tendon injuries are degenerative in nature and NOT inflammatory.
2. Anti-inflammatory medications (NSAID’s) and/or corticosteroid injections can actually accelerate the degenerative process and make the tendon more susceptible to further injury, longer recovery time and may increase likelihood of rupture.
3. Heavy load eccentric strength training helps to increase the tensile strength of the tendon, increase the amount of Type I collagen and decrease the amount of ground substance thereby reducing tendon volume and helping restore the tendon to a healthy state.
References:
Alfredson, H., Pietila, T., Jonsson, P., Lorentzon, R. Heavy-Load Eccentric Calf Muscle Training For the Treatment of Chronic Achilles Tendinosis. AJSM. Vol. 26 (3), 1998. pp.360-366
Cook, JL., Khan, KM., Maffulli, N., Purdam, C. Overuse Tendinosis, Not Tendinitis: Part 2: Applying the new approach to patellar tendinopathy. The Physician and Sportsmedicine, Vol 28 (6), June 2000.
Khan, KM., Cook, JK. Overuse Tendon Injuries: Where does the pain come from? Clinical Sports Medicine
Khan, KM., Cook, JL., Kannus, P., Maffulli, N., Bonar, SF. Time to abandon the “Tendinitis” Myth: Pianful, overuse tendon conditions have a non-inflammatory pathology. BMJ. Vol. 324 16 March 2002. pp.626-627.
Khan, KM., Cook, JL., Taunton, JE., Bonar, F. Overuse Tendinosis, Not Tendinitis: Part 1: A new paradigm for a difficult clinical problem. The Physician and Sportsmedicine, Vol 28 (5), May 2000.
Khan, KM. Cool, JL., Bonar, F., Harcourt, P., Astrom, M. Histopathology of Common Tendinopathies: Update and implications for clinical management. Sports Medicine. Jun 27 (6), 1999, pp. 393-408.
Kraushaar, B., Nirschl, RP. Tendinosis of the Elbow (Tennis Elbow). The Journal of Bone and Joint Surgery. Vol 81-A (2), Feb. 1999.
Maffulli, N., Ewen, SWB., Waterston, SW., Reaper, J., Barrass, V. Tenocytes from Ruptured and Tendinopathic Achilles Tendons Produce Greater Quantities of Type III Collagen than Tenocytes from Normal Achilles Tendons: An in vivo model of human tendon healing. AJSM Vol 28 (4), 2000.
Shalabi, A., Kristofferson-Wilberg, M., Svensson, L., Aspelin, P., Movin, T. Eccentric Training of the Gastrocnemius-Soleus Complex in Chronic Achilles Tendiopathy Results in Decreased Tendon Volume and Intratendinous Signal as Evaluated by MRI. AJSM, Vol. 32 No. X, 2004
Disclaimer
This information is not intended to be a substitute for professional medical advice. You should not use this information to diagnose or treat a health problem or disease without consulting with a qualified health care provider. Please consult your health care provider with any questions or concerns you may have regarding your condition.Any attempt to diagnose and treat an illness using the information in this site should come under the direction of a trained medical practitioner. We accept no responsibility for any adverse effects or consequences resulting from the use of any of the suggestions or procedures in this site or related internet links. By using the information in this web site you are confirming that you understand this statement and that you accept all risk and responsibility.
All matters regarding your health should be supervised by your health care provider. All information provided in this site is for the purpose of education, not treatment.

5 Comments:
thanks
hi used from it.
Many experts now see inflammation as arising from an immune system response that’s out of control. When you catch a cold or sprain your ankle, your immune system switches into gear. Infection or injury trigger a chain of events called the inflammatory cascade. The familiar signs of normal inflammation — heat, pain, redness, and swelling — are the first signals that your immune system is being called into action.
Inflammation symptoms
Thanks for the nice post. Do you know about ?? B-CURE LASER LLLT-808 - a breakthrough in soft laser therapy for efficient treatment of pain, wounds, burns,sports injuries, inflammation, acne, and laser therapy.
That is amazing. Joining the community is for the best and good for the family.
Sports Injuries in Monaghan
Post a Comment
<< Home